A diagnosis of prostate cancer is shocking and most often quite unexpected…the thought of a tumour growing inside you is sickening.
But I urge patients not to be so hasty. Mounting evidence shows that surgery is not always the best treatment.
Almost all men who have their prostate removed will suffer complications – whether that’s just slight incontinence, or the permanent erectile dysfunction experienced by around one in two.
If this were a guaranteed lifesaving operation, the risk might be worth it, but for many men, we now know their cancer is so slow-growing that it will never spread and there are good alternative options.
SURGERY DOES NOT IMPROVE SURVIVAL
The Prostate Intervention Versus Observation Trial (PIVOT) that began in 1994 included 731 men with an average age of 68 who had been diagnosed with the cancer.
Half of the men underwent surgery to remove the prostate – known as ‘radical prostatectomy’ – the others did ‘watchful waiting’, which means they had no immediate treatment.
Instead, they received hormone therapy if symptoms, including difficulty urinating, started to develop. The results showed that on average those who underwent surgery were no more likely to survive than the watchful waiting group.
Just seven per cent in the trial died of prostate cancer, compared with 41 per cent who died of unrelated conditions.
So, who should have surgery? Famous men who have faced this diagnosis – Hollywood actor Robert De Niro and South Africa’s Nelson Mandela spring to mind – have opted for an operation. But not all of the 30,000 Australian men diagnosed each year should do likewise.
BUT THERE ARE EXCEPTIONS
Men with prostate cancer frequently have no symptoms at all. The diagnosis is often made following prostate-specific antigen (PSA)
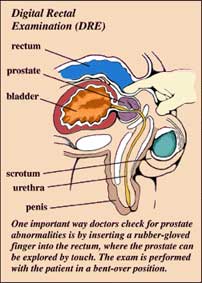
Men will also undergo a digital rectal examination to feel if the surface of the prostate has become lumpy.
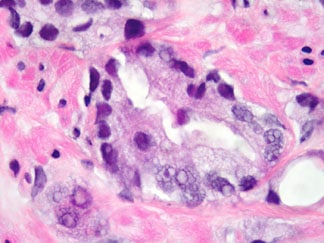
If the PSA levels are high or a change has occurred to the surface of the prostate, a biopsy is performed by taking tissue from the prostate with a needle.
The cancerous cells are examined under the microscope and a figure known as the Gleason score is calculated – the lower the score, the less likely the cancer will spread.
If results come back with a PSA score above 20 or a Gleason score between 8 and 10, it is usually advisable to have immediate treatment.
One thing PIVOT has highlighted is how much surgery appears to help those with high risk cancer.
ACTIVE SURVEILLANCE MAY BE THE BEST OPTION
In those diagnosed with a PSA score lower than 10 and a Gleason score of 6, I would not normally advise surgery. Instead, I would usually recommend active surveillance – which is a halfway house between watchful waiting and surgery.
The patient undergoes regular testing – MRI scans, blood tests and biopsies – to monitor the cancer. If there is evidence the cancer is growing, treatment options are discussed – this does not necessarily mean surgery.
Radiotherapy, brachytherapy (internal radiotherapy, where small radioactive metal seeds are placed within the tumour) and ultrasound treatment can be considered instead.
Watchful waiting is an option for those who are very elderly or who have other serious medical problems.
It is important that a man who has been diagnosed with low-risk prostate cancer overcomes the psychological hurdle that he has a cancer inside him.
Indeed, many specialists believe a Gleason 6 prostate tumour should not be termed as a ‘cancer’ at all because it differs enormously from the aggressive types – such as brain tumours – that spring to mind when the word ‘cancer’ is used.
Whether you suffer from low or high-risk cancer, there should be regular dialogue between your doctor, oncologist, urologist and yourself.
Don’t be overwhelmed by the mass of literature you are handed about the condition. Take time to think over the options available to you as removing the prostate is a life-changing course of action.
by David Livingstone

